INTRODUCTION
Myasthenia gravis is an autoimmune neuromuscular disorder, where in the receptors of the post synaptic membrane of the neuron gets affected by losing its ability to detect the presence of acetylcholine release from the presynaptic membrane of the neuron. It causes muscle weakness because of the inability of the neuromuscular junction to transmit enough signals from the nerve fibres to the muscle fibres.
PATHOLOGICAL CHANGES IN MYASTHENIA GRAVIS
Pathologically, antibodies that attack the acetylcholine receptors have been demonstrated in the blood of most patients with myasthenia gravis.
A. Normal neuromuscular junction – The nerve fibre forms a complex of branching nerve terminals that invaginate into the surface of the muscle fibres but lying outside the muscle fibre plasma membrane. The entire structure is called motor end plate.

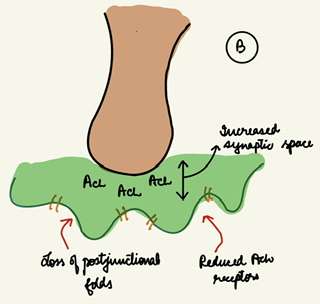
B. Changes in myasthenia gravis – Loss of post junctional folds, increased synaptic space and reduced ACh receptors occurs. Thus, end plate potentials that occur in the muscle fibres gets too weak to initiate opening of the voltage gated sodium channels and thus muscle fibre depolarisation does not occur.
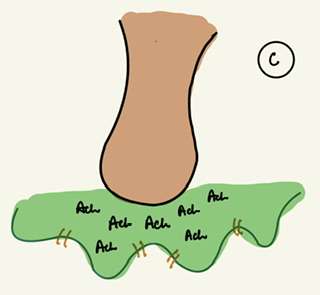
C. Effect of neostigmine in myasthenia gravis – The disease can usually be suppressed for several hours, by administrating neostigmine or some other anticholinesterase drug that allows larger than normal amounts of acetylcholine to accumulate in the Synaptic space.
SYMPTOMS OF MYASTHENIA GRAVIS
- Muscle weakness – It is the main symptom of the myasthenia gravis. This weakness can affect various muscles, including those involved in facial expression, eye movement, chewing and swallowing. Limb weakness can also occur in some cases.
- Fatigue and its affect – Central fatigue is highly prevalent in myasthenia gravis. This fatigue can impact both physical and mental activities.
- Diplopia (Double vision) – Weakness in the muscles controlling eye moment can lead to double vision.
- Ptosis (Drooping eyelids) – Weakness in the muscles responsible for lifting the eye lids can lead to ptosis causing one or both eyelids to droop.
- Speech and swallowing difficulty– Weakness in the muscles involved in speech can lead to slurred speech. Weakness in the muscles responsible for swelling can cause difficulty in chewing and swallowing food.
- Respiratory muscle weakness – In severe cases, myasthenia gravis can lead to weakness in the respiratory muscles, causing difficulty in breathing.
DIAGNOSIS
- Electromyography (EMG) and nerve conduction studies – EMG involves the insertion of the needles into specific muscles to record electrical activity during contraction and at rest. No conduction studies assess the speed and efficiency of nerve signals.
- Blood tests – measurement of specific antibodies associated with my senior gravis such as anti-acetylcholine receptor antibodies (AChR antibodies) or anti-muscle specific kinase antibodies (MuSK antibodies).
- Imaging studies to assess thymus abnormalities – Computed tomography (CT) or magnetic resonance imaging (MRI) may be used to examine the thymus gland, especially if thymoma is suspected.
- Tensilon Test – The Tensilon test involves the administration of a short acting acetylcholinesterase, inhibitor called edrophonium (Tensilon) intravenously.
TREATMENT
- Thymectomy – It is the surgical removal of the thymus gland. Thymectomy aims to modify the immune system is response and improve symptoms.
- Medications – Acetylcholinesterase inhibitors like physostigmine and neostigmine enhance the availability of ACh. Immunosuppressive medications like prednisone help modulate the immune response.
- Plasmapheresis – Plasmapheresis involves removing and replacing the liquid portion of the blood plasma, which contains antibodies that contribute to autoimmune response.
- Supportive Measures – Assistive devices such as eye glasses with reasons for double vision, speech therapy and physical therapy is generally recommended.
LIVING WITH MYASTHENIA GRAVIS
Living with myasthenia gravis is a unique journey, marked by resilience, adaptation and the daily triumphs for those who navigate its challenges.
- Navigating Daily Challenges – Strategically planning activities to conserve energy and minimise fatigue and assistive devices such as mobility aid can make daily tasks more manageable.
- Building a support system – Family and friends and connecting people who share similar experiences, play a crucial role in emotional and practical aspects of living with myasthenia gravis.
- Adapting Work and Daily Routine – The work arrangements should be flexible and self care like regular breaks and mindfulness should be prioritised.
- Communication Strategies – Transparent communication with healthcare professionals is very important.
FOR ANATOMY SECTION VISIT – https://medmaps.in/category/notes/anatomy/
GET CONNECTED TO US ON OUR INSTAGRAM PAGE – https://www.instagram.com/medmaps.in/
0 Comments